Children and adolescents affected by the drug crisis have acute and immediate needs that are different from adults. Think Kids is collaborating with community partners on a ground-up approach to identifying, articulating, and responding to these needs.
If you live in Boone, Clay, Fayette, Kanawha, Lincoln, and Putnam Counties, we need your help.
At the heart of our nation’s opioid epidemic lies West Virginia, and in the middle of this crisis are its children. The increase in parental substance abuse, impaired parenting, incarceration, extended separation from parents, overdose deaths, and introductions into the child welfare, court, and foster care systems have resulted in a children’s health crisis in our state.
For these children, adverse childhood experiences (ACEs) are highly prevalent and associated with a heightened risk of poor health outcomes in childhood and adulthood. Yet West Virginia’s response to the drug epidemic has been a patchwork of reactionary, adult-focused programs and services that have been systemic, siloed, and do not address the health care needs of affected children.
This project aims to assess how communities are responding to the unmet health care needs of children affected by the drug crisis.

We appreciate the Greater Kanawha Valley Foundation for supporting our work to address the unmet needs of children/adolescents affected by the drug epidemic.
Project Updates
Our end-of-year project report is out! Read below, share, or download. Thanks to all who worked with us in 2023. Your contribution is very much appreciated.
Naloxone saves lives from opioid overdoses, but only when it’s in the right place at the right time.
Should schools carry naloxone? That’s a decision left mostly in the hands of county school systems. Go here for a list of county school system naloxone policies in the project service area

We’re grateful to have had investigative reporter Amelia Knisely and videographer Tijah Bumgarner working with us in 2023. They will be interviewing community members about their experiences with substance use disorder and sharing their stories.

Tijah Bumgarner is a filmmaker and professor who teaches narrative and documentary video production at Marshall University. She holds a BFA in film/video from the California Institute of the Arts and a master’s degree in Media Studies from West Virginia State University. In 2017, Bumgarner completed her first feature film, Meadow Bridge, a coming-of-age narrative set in rural West Virginia. Most recently, her film
Picture Proof chronicles everyday moments in the life of one family in West Virginia as they rebuild, repair, and extend their life in the aftermath of substance use disorder.
We were fortunate to have Tijah join us this year as a contributor for this project, creating short films about people in recovery and those working in West Virginia communities to support them.

You can watch 25 films from multiple interviews with parents in long-term recovery and organizations supporting them on Tijah’s playlist on our YouTube channel.

Amelia Ferrell Knisely is an investigative reporter who has examined poverty and its ramifications in West Virginia for several publications, including the Charleston Gazette-Mail, Mountain State Spotlight, West Virginia Public Broadcasting, and now with West Virginia Watch. She has written extensively about homelessness and poverty and previously served as editor of The Contributor, a nonprofit newspaper sold by people experiencing homelessness. Originally from West Virginia, Amelia started her journalism career as a freelance journalist in her hometown. She holds a B.A. from Shepherd University and a master’s degree from Marshall University.
Amelia’s stories on our blog:
– In West Virginia’s mental health care desert, a health center focuses on providing help in schools

Dr. Sam Workman, Director, WVU Institute for Policy Research and Public Affairs, John D. “Jay” Rockefeller School of Policy and Politics worked with us on the assessment component of the project and wrote a final report about it titled Services for Families and Children in the Greater Kanawha Valley. You can download the full report or executive summary on our project cloud file.

Are services available in your county? Assessing accessible, affordable resources to help kids affected by familial drug use
By services, we mean: health care, mentoring, social support, and community resources that address social determinants of health, like food insecurity. Too often, we point people toward services that are miles away, are no longer in operation, or have restrictive service guidelines.
And yet, when we talk to policymakers, we lack the ability to articulate and prioritize where the need is greatest— where to strategically allocate funding and resources.
This year, we took a deeper dive into the landscape of community services for the Responding to the Needs of Kids Affected by the Drug Crisis project. Do kids really have access to meaningful services in their communities?
Our conclusion: Sometimes.
The above graphic is the final data visualization of the spreadsheet we shared with this email list a few weeks ago. We appreciate the expertise of Dr. Samuel Workman, a WVU professor and director of the Institute for Policy Research and Public Affairs in the John D. “Jay” Rockefeller IV School of Policy and Politics.
This graphic represents whether programs, services, and resources are available within each of the following counties: Boone, Clay, Fayette, Kanawha, Lincoln, and Putnam– TGKVF service area.
Before we assume that a program or service is available and accessible for children and youth, we need to take a harder look around our communities to see if services are available and accessible to those without the financial means to access them.
If services are unavailable, we should prioritize our advocacy efforts to ensure they’re available.
If services are available, we should promote them! We can begin by centralizing this data in WV 211 and ensuring those working directly with kids and families— social workers, health care providers, school staff, afterschool and childcare workers, etc.— are pointing families in this same direction.
There’s much we can do. Many thanks to those who worked with us on this project this year. We have posters and flyers of the data visualization available and are happy to send them to you.
Watch our project playlist on YouTube:
If you live in Boone, Clay, Fayette, Kanawha, Lincoln, or Putnam Counties, we can request free copies of our 2020-2021 report, From the Ground up: Addressing the Unmet Needs of Children Affected by the Drug Crisis. Complete the form below. You can also read it online or download it here.
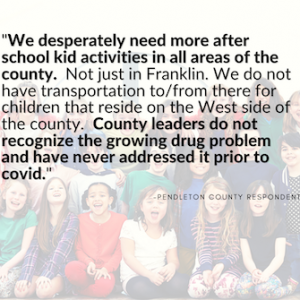
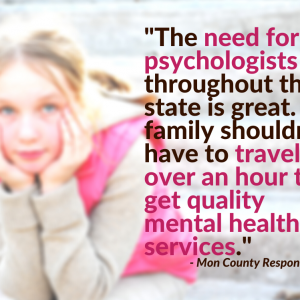
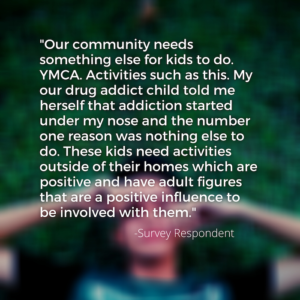
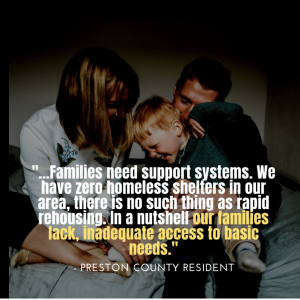
Participant Quotes: