Next week, we’re kicking off the Health and Hunger Summit series. During these months of planning, not being an expert in this field, I’ve made a note of observations and questions that I hope we dig into as the dialogue unfolds. Here are a few.
I’ve been a health advocate for a while, and I’ve worked peripherally on nutrition issues in a number of ways. For example, I was a member of the Mountains of Hope Cancer Coalition for years on their prevention subcommittee. We talked about good nutrition a lot, but we didn’t talk a lot about food insecurity or food deserts. Why does public health discuss proper nutrition without addressing the elephant in the room– that a growing number of us either have no access to or can’t afford nutritious food? Do they not recognize the breadth of the problem, or do prevention programs believe that tackling food insecurity is something for those who address economic stability, like within the framework of Healthy People 2030?
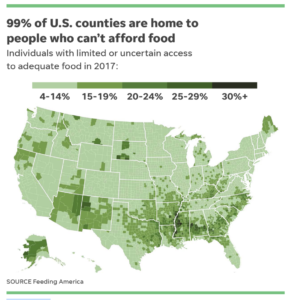
I remember after the 2016 flood, a few counties in my area lost their grocery stores. Families started relying on Dollar Generals and gas stations as food sources. I didn’t realize how prevalent this type of scenario was in our state until then. Take a look at these two graphics:
Just this week, The Trust for America’s Health released the State of Obesity: Better Policies for a Healthier America. On the right are the states with the highest pediatric obesity rates, including West Virginia. On the left is a map of self-reported data from those who identify themselves as sometimes or often lacking access to adequate food. I see a lot of overlap between counties where there’s a lack of adequate food and childhood obesity.
How can that be? Is this because children resort to eating sugary, over-processed food? I’d really like to learn more about that.
I’m eager to listen to the perspectives of those in the field– health care providers and those who manage food pantries around the state. It’s easy to say that all primary care providers should screen for food insecurity, but there are a host of valid reasons why many don’t– like not enough time, no care coordinator or social worker to help connect to resources or no resources in the community, and perhaps stigma– are people too ashamed or proud to share that they’re hungry? Is that something that advocates can work on?
Lastly, my biggest questions lie with the infrastructure in our state to address food insecurity. What role does state government play in ensuring that our system to address hunger is strong, sustainable, and increasing its reach? From conversations with pantry providers, it seems to me as if the faith-based community plays a much larger role than the state does. Years ago, I remember when the Center for American Progress published The Case for State Food Action Plans. I wonder if any states created plans, and if they’ve made progress? Some states are working on or have passed legislation to address hunger? What about here in our state legislature? Is there an interest? Do we have champions?
Here’s how I’m coming to this issue, as I prep for next week. The conversation kicks off on Tuesday at 10am. You can learn more and register on our website. Would love to hear your thoughts in the comments below.





0 Comments